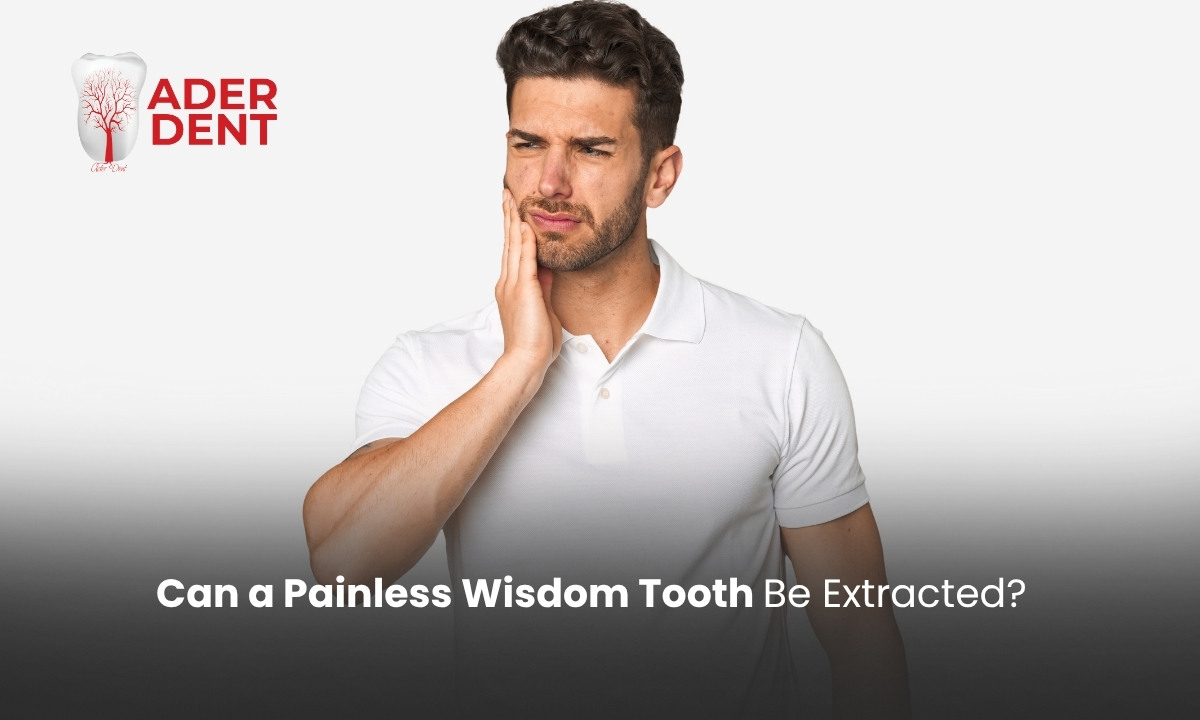
Infected teeth are caused by infections resulting from tooth decay or gum diseases. So, can an infected tooth be extracted, and what happens if it is? An infected tooth can be extracted, but the infection must first be brought under control. Extraction performed before the infection is treated can lead to the spread of infection and a prolonged healing process. Properly treated extractions, however, allow for faster recovery and prevent serious complications. Otherwise, problems such as throbbing tooth pain, persistent swelling, and severe discomfort become inevitable.
What Is an Infected Tooth?
An infected tooth is an infection that occurs in the tooth’s inner tissue (pulp) or surrounding root area. Deep cavities, gum diseases, and trauma to the tooth are the main causes of this infection. As the infection progresses, microorganisms accumulate at the tip of the root, causing swelling, throbbing, and pain in the gums. In some patients, the infection can become so severe that even normal daily activities become difficult.
Healing after an infected tooth extraction typically takes 7–10 days. Pain, swelling, and sensitivity during the first 24 hours are normal. During this period, hard, sticky, or extremely hot and cold foods should be avoided. Wisdom tooth infections are among the most common infected tooth issues. For symptoms like pain and swelling after a wisdom tooth extraction, you can check our article on post-wisdom tooth extraction infection symptoms.
Is Infected Tooth Extraction Risky?
Extraction of an infected tooth carries some risks. During extraction, the infection may spread to surrounding tissues or enter the bloodstream. Post-extraction swelling and pain may be higher than normal, and there is an increased risk of a dry socket. Additionally, the acidic environment in infected areas can reduce the effectiveness of local anesthesia, which may make the extraction more painful.
For this reason, dentists often prescribe antibiotics before extraction and perform the procedure under sterile conditions.
Will the Infection Spread After Tooth Extraction?
If the correct treatment is applied, the infection will not spread after the extraction, and the healing process will progress healthily. When an infected tooth is extracted properly and the dentist’s recommendations are followed, the risk of infection spreading is prevented. Antibiotic treatment before extraction is essential to control the infection.
Post-extraction hygiene and adherence to prescribed medications prevent the infection from spreading to surrounding tissues. Sterile conditions and proper care by a specialist dentist ensure that the infection does not spread after extraction.
Does Infected Tooth Extraction Hurt?
Extraction of an infected tooth is painless with appropriate local anesthesia. The main challenge in extracting an abscessed or infected tooth is that the area may not respond adequately to anesthesia, and the tooth can be extremely sensitive. This makes the dentist’s procedure more difficult and may increase pain during anesthesia. Therefore, even if extraction is planned, the decay or infected tissue causing the abscess must first be treated to control the infection, making the procedure safer and more comfortable.
What Happens If an Acutely Infected Tooth Is Extracted?
If an acutely infected tooth is extracted, the risk of rapid infection spread increases. Even if the infected tissues are cleaned, the infection may enter the bloodstream due to acute inflammation, potentially causing more serious health issues. For detailed information about symptoms of such infections, you can refer to our tooth root infection symptoms article.
In cases of acute infection, antibiotics are first administered to control the infection, followed by tooth extraction. This approach reduces the risk of infection spreading and ensures proper healing.
Can an Infected Tooth Be Extracted Without Antibiotics?
An infected tooth should not be extracted without antibiotics. The primary reason is to prevent the infection from spreading to other parts of the body during or after extraction.
Proper antibiotic use reduces the bacterial load in the infected area, making the procedure safer and more comfortable. However, in some cases, if the infection is mild or in an early stage, a dentist may perform the extraction without antibiotics. This decision is made by the dentist based on the patient’s health, severity of infection, and local findings.
Differences Between Acute and Chronic Tooth Infections
There are five main differences between acute and chronic tooth infections:
- Onset and pain: Acute infections start suddenly, intensify quickly, and cause throbbing pain. Chronic infections develop slowly and cause mild but persistent pain.
- Redness: The infection site in acute cases is clearly red. In chronic infections, redness is less pronounced.
- Systemic symptoms: Fever and fatigue may accompany acute infection; chronic infections usually have no systemic symptoms.
- Spread and tissue damage: Acute infections spread quickly and damage surrounding tissues, whereas chronic infections progress slowly and cause long-term damage.
- Urgency: Acute infections require urgent intervention as they can quickly harm oral health. Chronic infections progress silently but can cause permanent damage over time.
Post-Extraction Infection Treatment and Healing
Post-extraction infections can be quickly controlled with proper treatment and care. Antibiotic therapy, as recommended by your dentist, is crucial to prevent the infection from spreading. Pain relievers help reduce discomfort, and cold compresses applied during the first 24–48 hours alleviate discomfort at the extraction site.
Maintaining oral hygiene accelerates healing; therefore, gentle brushing without disturbing the extraction site is essential. Additionally, soft, non-sticky, and warm foods prevent irritation in the area. Avoiding smoking and alcohol is also highly important to support recovery and reduce the risk of infection.

 TR
TR